What is an Oral Aversion? Why does our baby have a feeding tube?
Babies born with CDH typically require a breathing tube for extended periods of time, additionally their digestive organs are not in the typical place even after repair surgery. This means the sucking and swallowing reflex is not as natural for children born with CDH as they are for children born typically healthy. Feeding issues are the problem that parents of children born with CDH report most often to us. These issues present while in the NICU and can follow CDH families for years. Reflux is also a common issue reported by parents. The inability to eat orally due to intubation combined with the reflux often leads to the development of severe oral aversion.
What is an oral aversion? According to WebMD, Oral aversion is when a child doesn’t want to eat or allow anything to touch their mouth. Children with oral aversion will avoid all food or just foods of certain types and textures. Serious cases of oral aversion can lead to nutrition problems.
So how do babies/children with oral aversions eat?
Parents who have children with oral aversions try to feed their children orally as instructed by their physician and speech/feeding therapist. This can be a frustrating experience for parents and babies. It can also be very stressful and heartbreaking for parents who often have feelings of failure surrounding what should be a “normal” activity where parents/caregivers bond with their child.
Feeding tubes are a tool that some physicians/hospitals require before a child born with CDH can be released. In some cases, parents are given the choice of staying in the NICU longer to work on feeding or having a feeding tube so they can go home more quickly.
Parents tend to have a love/hate relationship with feeding tubes. Parents are grateful for the ability to keep their child well-nourished. They love the ease of giving their children meds through the tube so they never have to taste the flavors of the liquid meds. On the other hand, it is a constant struggle mentally and emotionally for parents. It’s a natural instinct for a parent to want to feed their child but be unable to do so. While parents love that modern medicine has given them a tool to ensure their babies are getting the nutrition they need to grow and thrive, they hate that they need this tool which further signifies the differences children born with CDH face.
Types of Feeding Tubes:
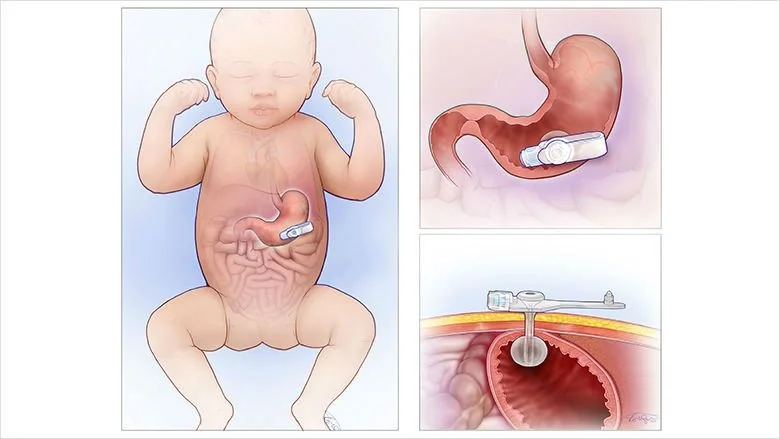
Gastrostomy Tube
To learn more about G-Tubes:
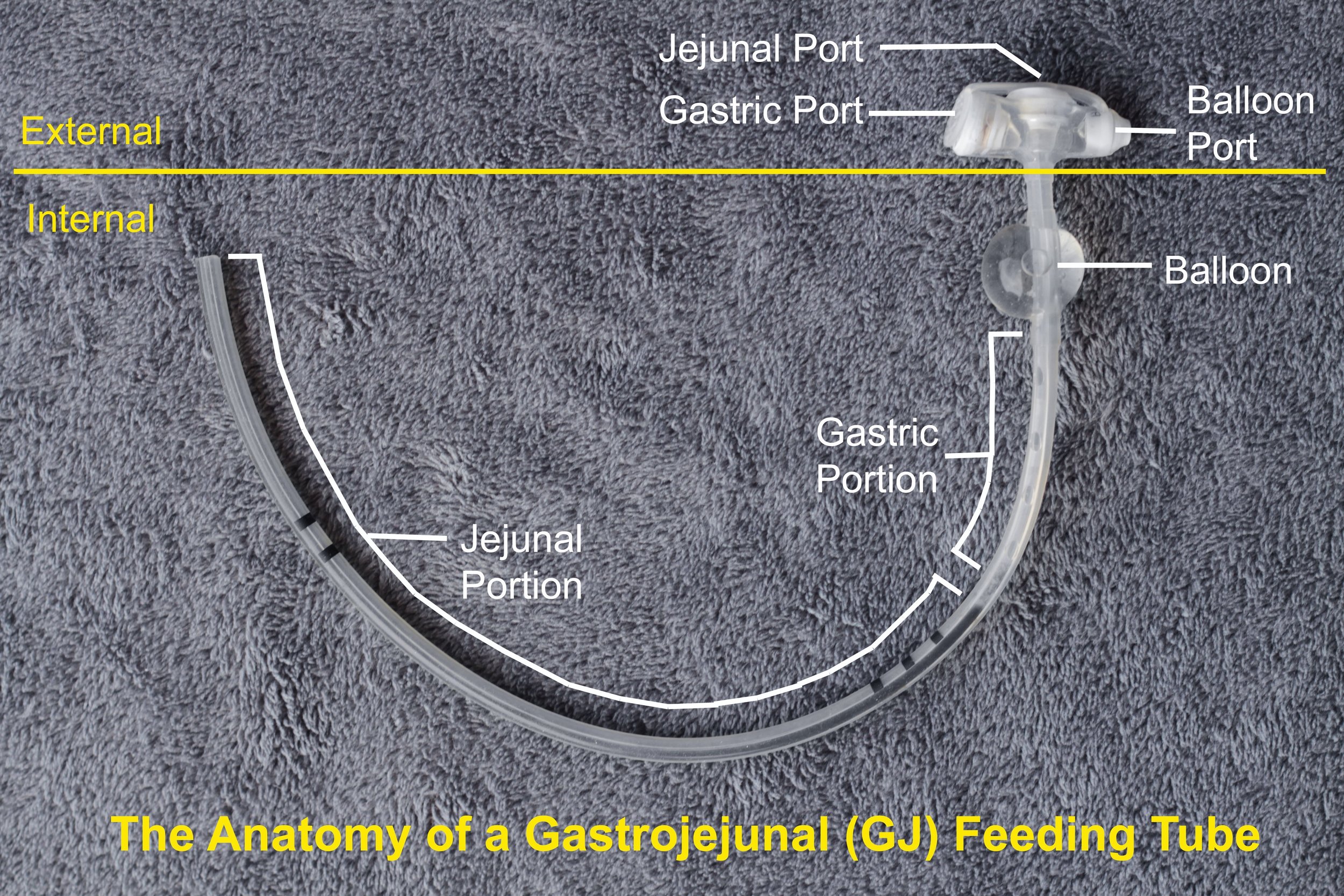
Gastrojejunal (GJ) Tube
To learn more about GJ-Tubes:
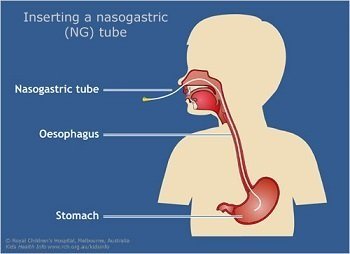
Nasogastric Tube
To learn more about NG- Tubes:
While these are the most common feeding tubes this is not an exhaustive list. If you would like more information please visit the link below:
How can I support a feeding tube family?
Never say a child with an oral aversion will eat by mouth if they get hungry enough. First, it is not true. Children with oral aversions will starve themselves instead of eating orally in most cases. Second, it is very hurtful to a parent whose child is struggling with an oral aversion.
Do not start a breastfeeding vs. formula feeding conversation with a parent whose child has an oral aversion/feeding tube, it is not helpful. Many moms whose children are tube fed pump breast milk and fortify it with high calorie formula to meet the nutritional needs of their child. A child with a feeding tube is under constant supervision from pediatricians, speech therapists, feeding therapists and nutritionists so parents of children with feeding tubes are actually making a more educated feeding decision than most. The CDH Foundation encourages all friends and family to adopt the mindset that “Fed is Best.”
Ask thoughtful questions. Parents are conscious of the fact that feeding tubes seem scary to others. Many parents report that friends and family members who ask questions make them feel loved and seen. Loved ones who shy away from acknowledging the feeding tube cause parents to feel both unloved and judged.
Parents of medically complex children often feel very isolated and alone. Close friends and grandparents can learn as much as possible about the feeding tube so that they can provide an occasional respite for parents. Parents may initially say no to letting others tube feed their children, but if loved ones continue to educate themselves and show willingness to follow the directions parents give eventually parents may say yes. Life with a medically complex child is a learning curve for everyone. Showing parents you want to learn with them shows them how much you love their whole family.
If a parent or caregiver is doing a feed either in public, or openly at home, show compassion and ask questions. Most parents appreciate curiosity because it shows you care. Every parent or caregiver knows children need to eat when they are hungry. Tube fed babies cannot always wait until there is complete privacy, nor should they. A child needs to eat no matter how they are fed.
Don’t ask how long a child will require a feeding tube. The answer is almost always unknown and it makes both the parents and children self-conscious. Some physicians also keep a feeding tube in place even after a child begins eating orally because sometimes children born with CDH have setbacks with their physical health that could in turn cause a setback in feeding.
G-Tube pads
Born Tubie Heroes is owned and operated by Veronica and Angie Thompson-Crew. These fun G-Tube pads can be used in place of medical gauze to help with skin irritation and any potential leakage. Check out all they have to offer below.
The CDH Foundation thanks all CDH parents who contributed information to this resource page.